The Military Protocol That Could Save Nursing



The U.S. military figured out how to stop combat stress before it turns into PTSD. Three hospitals quietly adapted the same protocol for nurses—and the results suggest it could change the future of healthcare itself.
The timing couldn't be more urgent. Last year alone, 138,000 nurses left the workforce—a number reported by the CEO of the National Council of State Boards of Nursing (NCSBN), Phil Dickison, citing findings from the 2024 Nursing Workforce Study. Another 40% of nurses say they'll walk away within five years. These aren't just statistics; they're signs of a profession hemorrhaging faster than hospitals can replace it.
But here's what makes this moment different: Dickison himself has been clear about the solution.
Healthcare leaders need to listen to nurses and involve them directly in the creation of solutions, instead of relying on top-down mandates.
He's telling us not to wait for institutional approval—but to act. Managers will continue to throw pizza parties and celebrate monthly birthdays to distract us from the problem, but frontline staff know the truth: retention strategies are failing in real time.
Here's where the military enters the picture. Stress First Aid (SFA) was designed for soldiers in life-or-death environments where traditional mental health support wasn't enough. Combat medics and field nurses needed something simple, structured, and peer-driven—something that recognized stress early and stopped it from spiraling into PTSD.
If it works on the battlefield, the question isn't whether it can work in hospitals—it's why we're still waiting to implement it. The military didn't ask field medics to wait for committee approval to save lives. Dickison is telling nurses the same thing—stop waiting for institutional permission.
Nurses already operate under relentless stress: codes, understaffing, patient deaths, hostile families, moral injury. The military validated SFA under conditions that make hospital stress look miniscule by comparison.
And this isn't just about bedside RNs. Administrators, educators, and policymakers should take note: SFA isn't a "feel-good" wellness initiative. It's a survival protocol for the workforce that underpins the entire health system.
The reality is simpler than institutional resistance - most hospitals simply don't know this system exists yet. The American Nurses Foundation (ANF) understands that in healthcare, adoption requires evidence-based science. That's exactly what they're building through their pilot programs.
Research takes time and costs money, but it's essential. The ANF isn't treating this as a "feel good intervention" - they're establishing the rigorous data that will eventually drive systemic change across the profession.
But here's the thing: while the ANF methodically builds that evidence base through their pilot hospitals, individual nurses don't have to wait. The tool exists now. The expertise is available now. Nurses who get to work and have an overwhelming assignment can say to their peers I’m yellow, and their colleagues would understand and provide support. This can happen today.
Some day, institutional transformation will come - backed by solid evidence. But personal professional development doesn't have to wait for the research cycle to complete. Every month of delay costs more in turnover than implementation would. Recruiting, onboarding, and training a single nurse can cost tens of thousands of dollars. Multiply that by 138,000 nurses lost last year, and the financial hemorrhage dwarfs any conceivable risk of adoption.
This is exactly what Dickison was warning against—waiting for top-down solutions while the workforce collapses in real time. While hospitals continue to wait for the evidence to come, 40% of nurses plan their exit strategies.
SFA isn't another wellness seminar or a one-size-fits-all "resilience toolkit." It's a systematic, peer-to-peer approach built for the realities of frontline work.
Informal support already happens—venting in the break room, texting after a rough shift—but without structure, it often goes nowhere. Stress First Aid transforms those moments into intentional interventions. It's proactive rather than reactive. Instead of waiting for burnout to turn into resignation, nurses can stop the spiral before it ends a career.
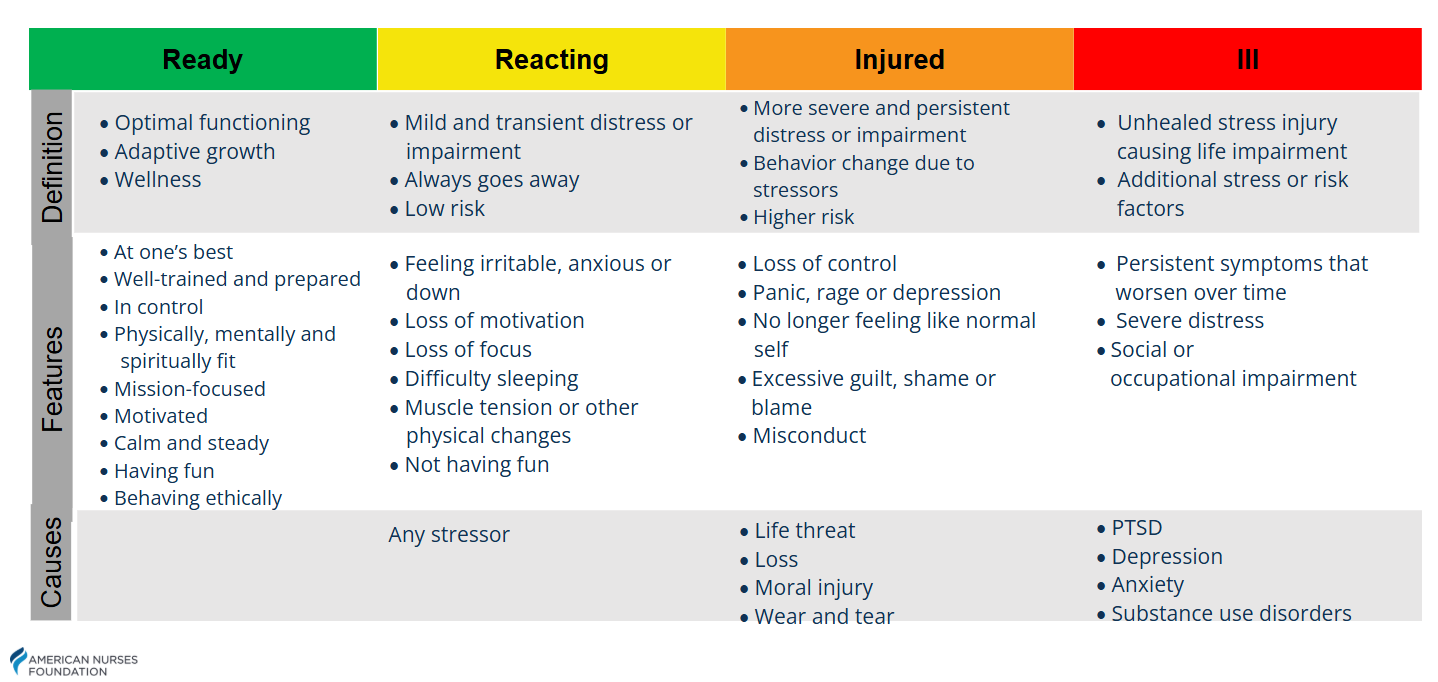
Stress First Aid builds on the Stress Continuum model, a simple color-coded spectrum originally designed by the military:
🟩 Green (Ready): functioning well, stable, coping.
🟨 Yellow (Reacting): temporary stress responses—irritability, trouble sleeping, fatigue.
🟧 Orange (Injured): stress is interfering with work or relationships—withdrawal, anxiety, intrusive thoughts.
🟥 Red (Ill): severe stress injury requiring professional help.
The power of the continuum is accountability. Nobody should end up in the red. If a colleague does, it means we missed earlier opportunities to recognize and respond when they were in yellow or orange. Red isn't failure of the individual—it's failure of the team to act.
But the continuum also sets boundaries. When someone is red, it doesn't mean nurses take on the role of therapist. It means the team escalates: connect that colleague to professional resources, involve EAP, and ensure they aren't left to navigate it alone. That clarity keeps peer support safe, structured, and sustainable.
Here's the irony: in most large health systems, you can't just hang up the Stress Continuum on the unit wall. It has to be cleared through the graphics department, then the area chief, and then a supervisor who may or may not think it's "appropriate." That's the kind of red tape nurses deal with when we try to help ourselves do our jobs better. And if you don’t have the right leaders in your unit, tools like this will never see the light of day.
This is exactly what Dickison was talking about. While administrators debate graphics approval, nurses are walking away. It's the quiet reality of nursing culture—still seen as inferior to physicians, still asked to stay in our lane, still expected to put our heads down and just do the work. And that stigma isn't just frustrating; it's costing the profession its future.
Yes, there are factors to manage:
But compare those to the current reality: 40% of nurses planning to leave. That's not a risk—it's a certainty unless something changes.
And here's the key: nurses are already informally supporting each other with zero training and zero boundaries. Stress First Aid doesn't add new responsibilities; it organizes what's already happening into a repeatable, clinically precise framework. Refusing to adopt it because it doesn’t comply with the hospital’s graphics committee is like rejecting a battlefield tourniquet because you're worried about leaving a scar. The wound is already bleeding out.
Here's the part most people don't know: the American Nurses Foundation (ANF) is currently offering Stress First Aid training at no cost. But only until 2027. That's a two-year countdown to equip ourselves with a tool that could extend nursing careers by years—or even save them outright. After that, access becomes uncertain.
The math is obvious. A few hours of training now versus tens of thousands in turnover costs later. Hospitals talk about ROI; it doesn't get any clearer than this. Waiting for more studies while free training expires is like watching an empty life raft drift away while the ship is sinking.
Nursing has never been about waiting for permission. We don't wait for committees when a patient codes. We don't wait for perfect data to start chest compressions. We act—because lives are at stake.
Dickison said it plainly: don't wait for top-down solutions. The CEO of nursing's regulatory body is giving you permission to act.
Stress First Aid deserves that same urgency. Every nurse knows a colleague teetering on the edge of burnout, or one who has already left. The next nurse we lose could be standing right beside you.
Here's what you can do now:
For nurses, this is about reclaiming agency. For hospital leaders, it's a business decision as much as a moral one. For educators, it's a chance to hardwire prevention into training before new grads ever touch a floor. And for patients, it's the reassurance that the people caring for you are cared for themselves.
The U.S. military proved Stress First Aid can save lives under the harshest conditions. The CEO of NCSBN has told us to stop waiting for institutional permission. If we can't act now to preserve our workforce, then when?
This isn't just a nursing issue. Administrators deciding on budgets, educators shaping curricula, and patients who want safe, consistent care all share the same stake. Stress First Aid is the rare intervention that's low-cost, evidence-informed, and immediately actionable across every level of healthcare.
The choice is here: act while the training is free and the profession can still be saved—or keep waiting for perfect data while the collapse accelerates. The profession that teaches healing has the power to heal itself.
References:
Dickison, Phil. CEO Interview on NCSBN CEO on How Nursing Can Move Forward as an Industry. American Nurses Foundation. May 25th, 2025. Available at: https://www.thenursinglens.org/resources/ or https://youtu.be/z0U7zgnLuiA?si=9fIOciuYS0HBmHT0